Full Version PDF
Chief Complaint
Left eyelid swelling and bruising
History of Present Illness
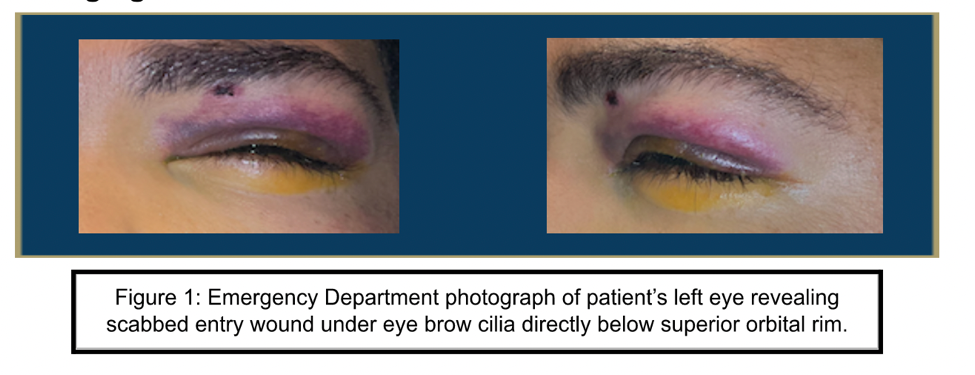
A 25-year-old male, with an unremarkable medical history, was transferred from an outside hospital after suffering a BB gun shot to his left orbit the preceding day. The patient recounted that he was standing approximately 10 feet from the BB gun. Immediately following the incident, he observed swelling and bleeding in his upper eyelid. He did not experience any alterations to his visual acuity. He denied flashes, floaters, diplopia, photophobia or ocular irritation.
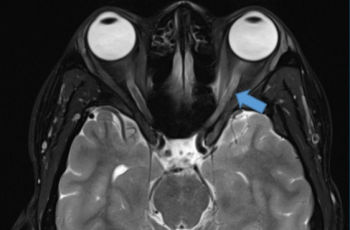
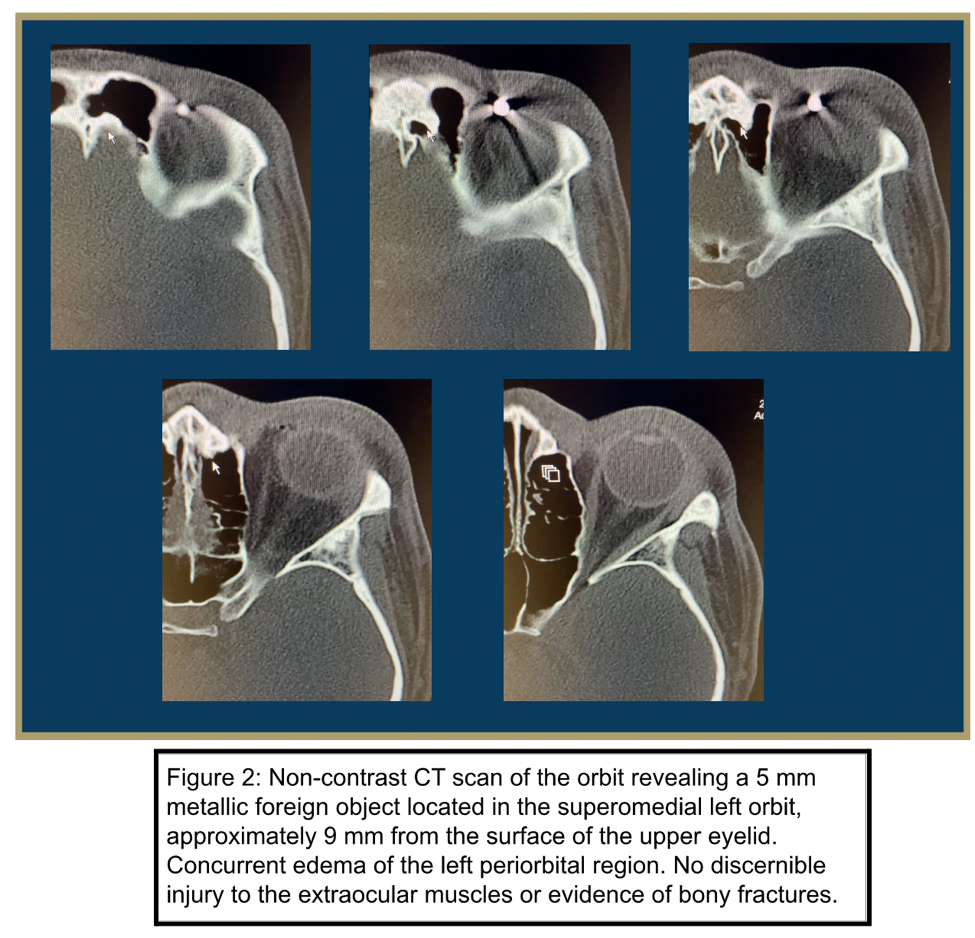
At the outside hospital, he received a single dose of IV antibiotics (ampicillin / sulbactam) and was subsequently transferred for ophthalmic evaluation. He denied vision changes but reported left eye swelling and bruising. A Computed tomography (CT) scan revealed a 5 mm foreign body located at the superior medial aspect of the left orbit, approximately 9 mm from the surface of the upper eyelid. There was no evidence of an injury to the globe. Tetanus vaccinations were up to date.
Ocular History
- None
Past Medical History
- None
Medications
- None
Allergies
- None
Family History
- None
Social History
- No relevant social history reported
Review of Systems
- All other systems within normal
Ocular Exam
Physical Exam
|
|
OD | OS |
|---|---|---|
| Visual Acuity | 20/20 | 20/20 |
| Intraocular Pressure (mmHg) | 11 | 10 |
| Pupils | PERRL no APD | PERRL no APD |
| Extraocular Motility | Full | Full |
Slit Lamp Exam
|
|
OD | OS |
|---|---|---|
| External | Normal | Scabbed entry wound under eyebrow cilia in medial limbal distribution directly below superior orbital rim. 1+ soft tissue edema and ecchymosis of the upper eyelid |
| Lids and Lashes | Normal, no lesions | Normal, no lesions |
| Conjunctiva/Sclera | White and quiet | White and quiet |
| Cornea | Clear | Clear |
| Anterior Chamber | Deep and quiet | Deep and quiet |
| Iris | Round and reactive | Round and reactive |
| Lens | Clear | Clear |
Dilated Fundus Exam
|
|
OD | OS |
|---|---|---|
| Cup to Disc | 0.7 | 0.7 |
| Optic Nerve | Pink/sharp | Pink/sharp |
| Vessels | Normal caliber/course | Normal caliber/course |
| Macula | Normal | Normal |
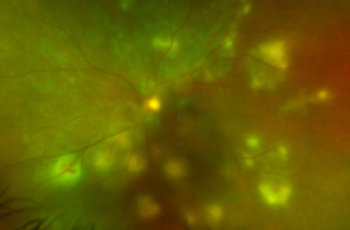
| Periphery | Attached 360; unremarkable | Attached 360; small <1DD area of commotion retinae superonasally; no elevation/rupture/hemorrhage |
| Vitreous | Clear | Clear |
Imaging
Laboratory Testing
- None
Differential Diagnosis
- Left intraorbital metallic foreign body
- Left intraocular metallic foreign body
- Globe rupture
- Orbital fracture
Clinical Course
A 25-year-old male patient with no past medical history presented one day following trauma to the left eye after being shot by a gas-powered airsoft gun from 10 feet away with a metal BB. A CT scan revealed a 5 mm foreign object located at the superomedial aspect of the patient's left orbit, approximately 9 mm from the surface of the upper eyelid. His visual function remained intact and there was no demonstrable evidence of an injury to the globe. The patient was prescribed a ten day course of Augmentin and erythromycin 0.5% ointment applied to the entry wound four times daily. The foreign body was ultimately removed without complications
Discussion
An orbital foreign body can be defined as any extraneous object, either wholly or partially, occupying the orbital space. A comprehensive incidence study involving eye injuries treated in American Emergency Departments ascertained that foreign bodies were the leading causative agents, attributing to 44.3% of all cases.1 The foreign object may be present with or without globe penetration or perforation. Furthermore, the orbital foreign body can be categorized as either purely orbital or transorbital.
Injury to the orbital region due to foreign bodies is most commonly traumatic; however, instances of iatrogenic injuries have been documented, especially as a result of surgical orbital implants. A history of trauma, encompassing sport-related incidents, violence, battlefield injuries, or industrial accidents, is a significant risk factor for the occurrence of orbital foreign bodies. Studies also suggest a higher prevalence of these injuries among younger men.2–8
Consistent with our patient's case, ocular trauma primarily affects males, with a male-to-female ratio reported at approximately 6:1.4 The mean age of patients with ocular trauma varies, though one study reported it to be 36.0 ± 20.0 years.4 Most ocular injuries occur at home or within the workplace, with metal, glass, explosions, and intraocular foreign bodies being the common causes. It is estimated that about one-third of all ocular injuries could be preventable, with domestic accidents and children being the primary contributors.8
Factors associated with poor visual outcomes in ocular trauma cases include female gender, advanced age, specific injury types (e.g., zone III injury, eyelid injury), and the presence of intraocular foreign bodies.4 Post open globe injury repair, potential complications such as wound leak and endophthalmitis have been identified. Factors such as stellate-shaped wounds and delayed presentation contributed to wound leaks, while delayed presentation, microbial keratitis, and lens capsule breach were associated with an increased risk of endophthalmitis.
Maxillofacial computed tomography (CT) scan is the preferred imaging modality for evaluating and diagnosing intraocular foreign bodies.12 It's crucial to remember that while CT scans can help assess the presence of globe rupture, they should be seen as a supplement to an ophthalmic evaluation rather than a replacement for a physical exam.13 In situations like our present case where there's ferromagnetic ocular trauma, MRI is firmly contraindicated. Similarly, ultrasound is generally not employed to assess globe rupture due to concerns that direct pressure on the globe could exacerbate the injury.11 It should be noted that in select cases, ophthalmologists may elect to carefully perform ultrasonography without compressing the globe to complete the exam in a suspected globe rupture.
The decision to surgically remove intraorbital foreign bodies is driven by several considerations. The presence of a large or sharp-edged foreign body, indicative of potential further harm, necessitates removal. Signs of infection or inflammation, such as endophthalmitis, call for surgical intervention to manage the infection. Conditions like proptosis, restricted eye movement, chemosis, palpable orbital mass, and optic nerve compression are also strong indications for surgical removal. If imaging reveals an abscess or an enhancing foreign body, surgery becomes a requirement. Foreign bodies composed of wood, vegetable matter, or copper, given their higher risk of complications, should be removed. Fistula formation also mandates surgical intervention. These indications serve as guiding principles when deciding on the removal of intraorbital foreign bodies, although each case should be evaluated individually considering the patient's condition and the healthcare providers' expertise.1
The final visual outcome is prognosticated by the presenting visual acuity.11,14 Several other factors, including longer wound length, relative afferent pupillary defect vitreous prolapse, vitreous hemorrhage, posterior globe involvement, retinal detachment, endophthalmitis, and hyphema, have been associated with poorer post-injury visual acuity.15–18 Ophthalmologists treating a patient with severe ocular trauma can utilize the Ocular Trauma Score (OTS) to predict the prognosis of their post-injury visual acuity. The OTS scores range from 1 (most severe) to 5 (least severe) and take into account the factors mentioned earlier, with the initial (raw) score originating from the patient's presenting visual acuity.19
References
1. Al-Mujaini A, Al-Senawi R, Ganesh A, Al-Zuhaibi S, Al-Dhuhli H. Intraorbital Foreign Body: Clinical Presentation, Radiological Appearance and Management. Sultan Qaboos Univ Med J. 2008;8(1):69-74.
2. Finkelstein M, Legmann A, Rubin PA. Projectile metallic foreign bodies in the orbit: a retrospective study of epidemiologic factors, management, and outcomes. Ophthalmology. 1997;104(1):96-103. doi:10.1016/s0161-6420(97)30355-8
3. McGwin G, Owsley C. Incidence of emergency department-treated eye injury in the United States. Arch Ophthalmol. 2005;123(5):662-666. doi:10.1001/archopht.123.5.662
4. Hoskin AK, Low R, Sen P, et al. Epidemiology and outcomes of open globe injuries: the international globe and adnexal trauma epidemiology study (IGATES). Graefes Arch Clin Exp Ophthalmol. 2021;259(11):3485-3499. doi:10.1007/s00417-021-05266-1
5. Kong GYX, Henderson RH, Sandhu SS, Essex RW, Allen PJ, Campbell WG. Wound-related complications and clinical outcomes following open globe injury repair. Clin Exp Ophthalmol. 2015;43(6):508-513. doi:10.1111/ceo.12511
6. Nasr AM, Haik BG, Fleming JC, Al-Hussain HM, Karcioglu ZA. Penetrating orbital injury with organic foreign bodies. Ophthalmology. 1999;106(3):523-532. doi:10.1016/S0161-6420(99)90111-2
7. Fulcher TP, McNab AA, Sullivan TJ. Clinical features and management of intraorbital foreign bodies. Ophthalmology. 2002;109(3):494-500. doi:10.1016/s0161-6420(01)00982-4
8. Framme C, Roider J. Epidemiologie offener Augenverletzungen. Klin Monbl Augenheilkd. 1999;215(11):287-293. doi:10.1055/s-2008-1034716
9. Smith D, Wrenn K, Stack LB. The epidemiology and diagnosis of penetrating eye injuries. Acad Emerg Med. 2002;9(3):209-213. doi:10.1111/j.1553-2712.2002.tb00246.x
10. Hughes E, Fahy G. A 24-month review of globe rupture in a tertiary referral hospital. Ir J Med Sci. 2020;189(2):723-726. doi:10.1007/s11845-019-02097-2
11. Blair K, Alhadi SA, Czyz CN. Globe Rupture. In: StatPearls. StatPearls Publishing; 2023. Accessed May 10, 2023. http://www.ncbi.nlm.nih.gov/books/NBK551637/
12. Modjtahedi BS, Rong A, Bobinski M, McGahan J, Morse LS. Imaging characteristics of intraocular foreign bodies: a comparative study of plain film X-ray, computed tomography, ultrasound, and magnetic resonance imaging. Retina. 2015;35(1):95-104. doi:10.1097/IAE.0000000000000271
13. Chou C, Lou YT, Hanna E, et al. Diagnostic performance of isolated orbital CT scan for assessment of globe rupture in acute blunt facial trauma. Injury. 2016;47(5):1035-1041. doi:10.1016/j.injury.2016.01.014
14. Yeh S, Colyer MH, Weichel ED. Current trends in the management of intraocular foreign bodies. Curr Opin Ophthalmol. 2008;19(3):225-233. doi:10.1097/ICU.0b013e3282fa75f1
15. Yalcin Tök O, Tok L, Eraslan E, Ozkaya D, Ornek F, Bardak Y. Prognostic factors influencing final visual acuity in open globe injuries. J Trauma. 2011;71(6):1794-1800. doi:10.1097/TA.0b013e31822b46af
16. Meng Y, Yan H. Prognostic Factors for Open Globe Injuries and Correlation of Ocular Trauma Score in Tianjin, China. J Ophthalmol. 2015;2015:345764. doi:10.1155/2015/345764
17. Agrawal R, Wei HS, Teoh S. Prognostic factors for open globe injuries and correlation of ocular trauma score at a tertiary referral eye care centre in Singapore. Indian J Ophthalmol. 2013;61(9):502-506. doi:10.4103/0301-4738.119436
18. Lieb DF, Scott IU, Flynn HW, Miller D, Feuer WJ. Open globe injuries with positive intraocular cultures: factors influencing final visual acuity outcomes. Ophthalmology. 2003;110(8):1560-1566. doi:10.1016/S0161-6420(03)00497-4
19. Kuhn F, Maisiak R, Mann L, Mester V, Morris R, Witherspoon CD. The Ocular Trauma Score (OTS). Ophthalmol Clin North Am. 2002;15(2):163-165, vi. doi:10.1016/s0896-1549(02)00007-x
20. Lee SC, Park SH, Han SK, et al. Prognostic Factors of Orbital Fractures with Muscle Incarceration. Arch Plast Surg. 2017;44(5):407-412. doi:10.5999/aps.2017.44.5.407
Chief Complaint
Bilateral blurry vision
History of Present Illness
A 35 year-old male presented to the ophthalmology clinic with progressive worsening of his blurry vision for the past year. The patient reported experiencing sensitivity to bright lights and difficulty driving at night. However, he denied any ocular pain and only endorsed experiencing mild itching in both eyes. The patient reported no recent episodes of new flashes or floaters in his visual field.
Ocular History
- None
Past Medical History
- None
Medications
- None
Allergies
- None
Family History
- None
Social History
- No relevant social history
Review of Systems
- Noted in HPI, otherwise negative
Ocular Exam
Physical Exam
|
|
OD | OS |
|---|---|---|
| Visual Acuity | 20/30- | 20/40 |
| Intraocular Pressure (mmHg) | 22 | 21 |
| Pupils | PERRL no APD | PERRL no APD |
| Extraocular Motility | Full |
Full |
| Refraction | Plano +0.75 x 090 | +1.00 +0.50 x 120 |
| BCVA | 20/30 | 20/25- |
Slit Lamp Exam
|
|
OD | OS |
|---|---|---|
| External | Normal | Normal |
| Lids and Lashes | Normal, no lesions | Normal, no lesions |
| Conjunctiva/Sclera | White and quiet | White and quiet |
| Cornea | Clear | Clear |
| Anterior Chamber | Deep and quiet | Deep and quiet |
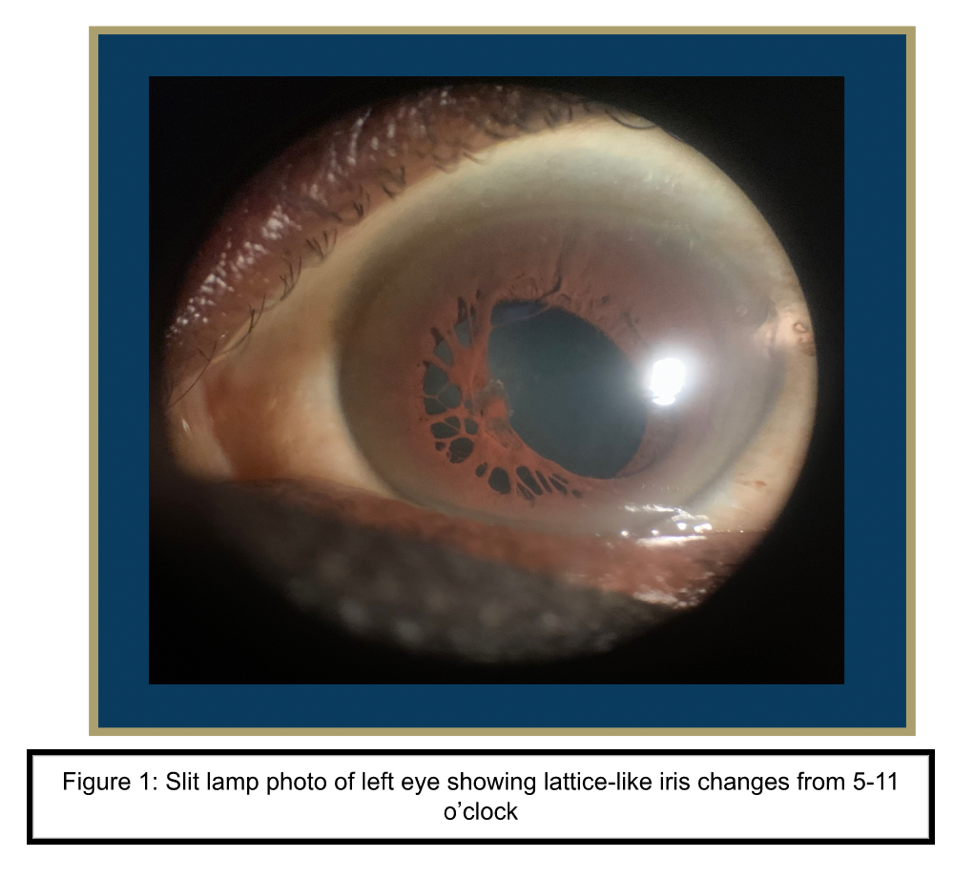
| Iris | Round and reactive, perilimbal nodules | Round and reactive, lattice-like iris change |
| Lens | Clear | Clear |
Dilated Fundus Exam
|
|
OD | OS |
|---|---|---|
| Cup to Disc | 0.3 | 0.3 |
| Optic Nerve | Pink/sharp | Pink/sharp |
| Vessels | Normal caliber/course | Normal caliber/course |
| Macula | Normal | Normal |
| Periphery | Flat, media clear, no other inflammatory retinal findings | Flat, media clear, no other inflammatory retinal findings |
| Vitreous | Clear | Clear |
Imaging
Differential Diagnosis
- Post-inflammatory synechiae
- Persistent Pupillary Membrane
- Congenital idiopathic microcoria
Clinical Course
A 35-year-old male presented to the ophthalmology clinic with worsening blurry vision for the past year. Refraction was performed and provided moderate visual improvement. Slit lamp exam revealed perilimbal iris nodules in the right eye and peripupillary lattice-like iris changes in the left eye. The anomalous iris changes were determined to be a persistent pupillary membrane. The patient’s reported nyctalopia was noted to be secondary to the iris changes.
Discussion
Persistent Pupillary Membrane (PPM) are congenital iris strands in the pupil. These strands are remnants of the anterior tunica vasculosa lentis which plays a critical role in delivering nutrients to the eye's lens during the initial six months of fetal development. The hyaloid vascular system, a vessel network formed during embryonic development to nourish the eye, usually dissolves around the third trimester. However, the failure of this natural process leads to PPM. It's noteworthy that these cases rarely remain vascularized, with only 0.3% exhibiting such traits.
PPMs hold the distinction of being the most frequent congenital anomaly, observed in nearly 95% of newborns, as per Tanzer's study in 1997.1 There's no identified demographic specifically prone to PPM. Since it generally doesn't affect visual acuity, there's no defined age for reporting this finding to an ophthalmologist. A unique case report has recently explored the connection between tetralogy of Fallot and PPM.2
Symptomatically, PPM varies from no discernable impact to significant reduction in visual acuity, particularly in bilateral cases. Pupillary apertures smaller than 1.55 can potentially disrupt light reaching the retina. Persistent vessels may degrade visual acuity by shrinking the pupillary aperture, as noted by Banigallapati in 2018.3 Additionally, PPM's association with other ocular anomalies such as cataracts, amblyopia, strabismus, and anterior segment abnormalities can also hinder visual acuity.4 If not addressed early, PPM can lead to amblyopia or 'lazy eye' due to a discrepancy between the brain and eye function.5
PPM are typically discovered during slit lamp examination. The examining ophthalmologist can observe a variety of types; from a few strands to a dense membrane reaching across the pupil and connecting at the collarette, a defining sign of PPM. Collarette refers to the iris line separating the central pupillary zone from the peripheral ciliary zone. Despite PPM, intraocular pressures generally remain within normal limits, with no other systemic findings observed.3 Optical coherence tomography imaging doesn't reveal any unusual findings as PPM primarily involves the pupil and iris. Other diagnostic tools including retinoscopy and iris angiography are useful to identify focal lens opacities and, in rare cases, vascular perfusion.
The majority of PPMs are asymptomatic, but if they fail to atrophy within the first year of life, they can cause visual impairment. In instances where they persist, surgical excision may be warranted. Mild PPM cases can be managed conservatively with mydriatics, refractive correction, and patching for amblyopia.6 More severe cases demand surgical excision of the pupillary membrane. However, this approach carries risks such as intraoperative bleeding and potential infection. Microsurgical scissors require a smaller working space in the anterior chamber and offer an edge over micro Vannas scissors in mitigating intraoperative complications. A retrospective study investigating long-term complications of surgical excision for treating PPM using vitreous scissors found that only 2 out of 24 patients exhibited long-term lens opacity.7
The Nd:YAG laser, which targets and destroys abnormal tissue, has also demonstrated effectiveness.8 The procedure involves disrupting the adhesion between the membrane strands and the normal iris collarette using an Nd:YAG laser, effectively displacing the membrane downward and clearing the visual axis.9 However, this method is not suitable for younger children or those with thicker pupillary membranes. Some studies recommend the Argon laser as an alternative to the Nd:YAG laser, citing the latter's propensity for causing pain, pigment dispersion, and bleeding.10
Femtosecond Laser-assisted Cataract Surgery (FLACS) has also been proven effective in addressing PPM in patients also suffering from cataracts (Kim JY, 2022).11 This procedure involves a three-step process: corneal arcuate incision, anterior capsulotomy, and lens fragmentation. It is considered superior to conventional cataract surgery due to its increased accuracy and reduced risk of intraoperative complications. A case study involving a 61-year-old female patient showed an improvement in corrected distance visual acuity (CDVA) from 0.3 preoperative to 1.0 one month postoperative, with no intraoperative complications reported.
The visual prognosis following early surgery is generally excellent, especially when complemented with visual rehabilitation. Researchers recommend early intervention and timely visual rehabilitation to achieve the best visual prognosis in patients with PPM.5 Although Vannas Scissors are effective, they carry the risk of general anesthesia, intraoperative bleeding, intraocular infection, and potential cataract induction if the lens is inadvertently damaged during pupillary membrane removal. This is why Vitreous Scissors, posing fewer risks to the patient, are the preferred choice.12
While the Nd:YAG laser has shown effectiveness in treating PPM, it carries risks of cataract formation, iritis, and pigment dispersion.3 A retrospective study on patients with hyperplastic PPM found that, out of 39 eyes in 24 patients, the average best corrected vision at the final appointment was 20/40, with only 5 eyes reaching a best vision of 20/70. Anisometropia, a condition characterized by asymmetric refraction between the two eyes, was found in only 11 of the 24 patients.7 Another potential complication is damage to the anterior lens capsule if the membrane adheres to the lens during PPM removal.4 Although PPM treatment is generally considered safe, these potential complications should be clearly communicated to patients.
In conclusion, Persistent Pupillary Membrane (PPM) is a common congenital anomaly characterized by fetal iris strands in the pupil. While most cases are asymptomatic, PPM can lead to visual impairment if it persists beyond the first year of life. Diagnosis is typically made through slit lamp examination, and treatment options range from conservative management to surgical excision. Different surgical approaches, such as microsurgical scissors, Nd:YAG laser, and Femtosecond Laser-assisted Cataract Surgery (FLACS), have been used, each with its own benefits and potential complications. Early surgical intervention combined with visual rehabilitation yields excellent visual outcomes, and ongoing research aims to further enhance PPM management.
References
1. Tanzer DJ, McClatchey SK. Spontaneous hyphema secondary to a prominent pupillary membrane in a neonate. J Pediatr Ophthalmol Strabismus. 1997;34(5):318-320. doi:10.3928/0191-3913-19970901-15
2. Chang M, Ancona-Lezama D, Shields CL. Vascular perfusion in persistent pupillary membrane of the iris. Indian J Ophthalmol. 2019;67(10):1704-1705. doi:10.4103/ijo.IJO_311_19
3. Banigallapati S, Potti S, Marthala H. A rare case of persistent pupillary membrane: Case-based approach and management. Indian J Ophthalmol. 2018;66(10):1480-1483. doi:10.4103/ijo.IJO_495_18
4. Altun A, Kurna SA, Bozkurt E, et al. Bilateral Persistent Pupillary Membrane with Tetralogy of Fallot: A Case Report and Review of the Literature. Case Reports in Ophthalmological Medicine. 2014;2014:e581273. doi:10.1155/2014/581273
5. Huang YT, Lin HJ. Long term surgical outcome for persistent pupillary membranes with associated ocular abnormalities: a retrospective case series study. BMC Ophthalmology. 2021;21(1):232. doi:10.1186/s12886-021-01990-8
6. Kurt E. A patient with bilateral persistent pupillary membrane: a conservative approach. J Pediatr Ophthalmol Strabismus. 2009;46(5):300-302. doi:10.3928/01913913-20090903-08
7. Lee SM, Yu YS. Outcome of hyperplastic persistent pupillary membrane. J Pediatr Ophthalmol Strabismus. 2004;41(3):163-171. doi:10.3928/0191-3913-20040501-09
8. Gupta R, Kumar S, Sonika null, Sood S. Laser and surgical management of hyperplastic persistent pupillary membrane. Ophthalmic Surg Lasers Imaging. 2003;34(2):136-139.
9. Oner A, Ilhan O, Dogan H. Bilateral extensive persistent pupillary membranes. J Pediatr Ophthalmol Strabismus. 2007;44(1):57-58. doi:10.3928/01913913-20070101-12
10. Ahmad SS, Binson C, Lung CK, Ghani SA. Bilateral persistent pupillary membranes associated with cataract. Digit J Ophthalmol. 2011;17(4):62-65. doi:10.5693/djo.02.2011.10.001
11. Kim JY, Jun I, Kim TI, Seo KY. Successful Femtosecond Laser-assisted Cataract Surgery for a Cataract with Persistent Pupillary Membrane: A Case Report. Korean J Ophthalmol. 2022;36(5):474-475. doi:10.3341/kjo.2022.0046
12. Lee HJ, Kim JH, Kim SJ, Yu YS. Long-term Lens Complications Following Removal of Persistent Pupillary Membrane. Korean J Ophthalmol. 2018;32(2):103-107. doi:10.3341/kjo.2017.0069
Acknowledgments
Case Report Authors
Case 1: Metallic BB Orbital Trauma
Madeline Rocks, MS1
Abood Salman, MS1
Case 2: Persistent Pupillary Membrane
Alain Greenwald, MS1
Siddhanth Iyer, MS1
Medical Student Editors
Yusuf Bade, BA MS1
Resident Editors
Masumi Asahi, DO
Will Foos, MD
Braedon Murdock, MD
Attending Reviewer
David Belyea, MD MBA
Keith Wroblewski, MD
Editors in Chief
Jason Dossantos, BS MS3
Julie Thomasian, BS MS4