Full Version PDF
Chief Complaint
Gradual painless vision loss in the left eye
History of Present Illness
28-year-old female with G6PD deficiency and otherwise unremarkable past medical history presents to the emergency department with 2-week history of painless, decreased vision of the left eye. Additionally, she reported a left sided headache for the first week and endorsed discomfort with left eye movement. She denied head trauma, fever, paresthesia, weakness, changes in hearing, tinnitus, pain when chewing, tearing, redness, or recent flu like symptoms. She recalled a similar episode of vision loss in the left eye that resolved in 3 weeks with no intervention approximately 4 months ago.
Ocular History
- None
Past Medical History
- G6PD deficiency
Medications
- None
Allergies
- No known drug allergies
Family History
- None
Social History
- Daily E-Cigarette use
Review of Systems
- As noted in HPI, otherwise negative
Ocular Exam
Physical Exam
|
|
OD | OS |
|---|---|---|
| Visual Acuity | 20/20 | CF |
| Intraocular Pressure (mmHg) | 13 | 12 |
| Pupils | Round, reactive | 2+ APD |
| Extraocular Motility | Full | Full |
| Color Plates | Full | Unable |
Slit Lamp Exam
|
|
OD | OS |
|---|---|---|
| External | Normal | Normal |
| Lids and Lashes | Normal, no lesions | Normal, no lesions |
| Conjunctiva/Sclera | White and quiet | White and quiet |
| Cornea | Clear | Clear |
| Anterior Chamber | Deep and quiet | Deep and quiet |
| Iris | Round and reactive | Round and reactive |
| Lens | Clear | Clear |
Dilated Fundus Exam
|
|
OD | OS |
|---|---|---|
| Cup to Disc | 0.3 | 0.3 |
| Optic Nerve | Pink/sharp | Pink/sharp |
| Vessels | Normal | Normal |
| Macula | Normal | Normal |
| Periphery | Flat | Flat |
| Vitreous | Clear | Clear |
Imaging
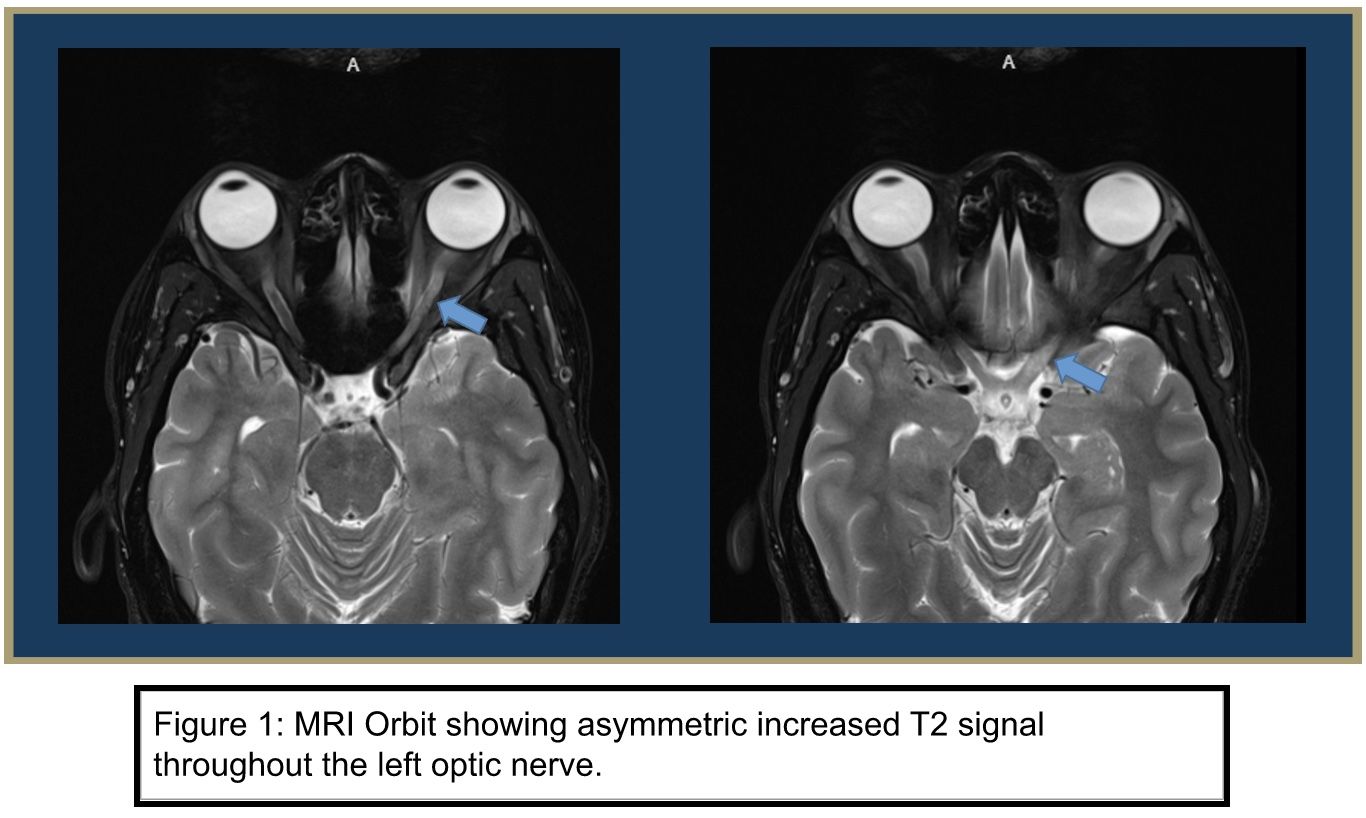
MRI Face/neck/orbit with and without contrast
Abnormal appearance of left optic nerve including prominent asymmetric increased T2 signal throughout the left optic nerve which appears most pronounced intracranially where there is also mild enlargement and prominent enhancement of the nerve which extends slightly into the left side of the optic chiasm. There is lesser enhancement of the orbital portion of the left optic nerve without apparent enlargement. These findings are indicative of acute optic neuritis. Normal MRI examination of the right optic nerve performed with and without contrast.
MRI Brain with and without contrast
There is a single high T2 signal intensity lesion in the left precentral gyrus suspicious for demyelinating disease given its appearance and location, particularly given the patient's clinical presentation and apparent left optic neuritis on the concurrent MRI examination of the orbits. The remaining brain is within normal limits.
MRI/MRV Head without contrast
Nromal MR venogram of the brain. Specifically, there is no evidence of dural venous sinus thrombosis
MRI Cervical Spine and Thoracic with and without contrast
Essentially normal MRI of the cervical and thoracic spine
Laboratory Testing
- ESR, CRP, IgG, HIV, ANA negative/unremarkable
- CSF Oligoclonal bands- positive (type 2)
- CSF ACE- negative
- NMO AQP4-IgG- negative
- MOG-IgG- negative
- CSF analysis: cell count 4WBC (89% lymphs), glucose: 89, IgG: 1,232
- CSF with cx: mild pleocytosis, normal protein, no polymorphonuclear lymphocyte
- CSF IgG index 1.6 (high), IgG synthesis rate 4.2 (high)
- Meningoencephalitis panel- negative
Differential Diagnosis
- Clinically isolated syndrome (CIS) of optic neuritis (ON) or prodromal of multiple sclerosis
- Neuromyelitis optica spectrum disorder
- Anti-myelin oligodendrocyte glycoprotein syndrome
- Lupus
Clinical Course
The patient is a 26-year-old female with a past medical history of G6PD deficiency who was
admitted for recurrent subacute left-sided visual loss with APD and contrast-enhancing left optic nerve on imaging, concerning optic neuritis. MRI of the brain showed central vein sign
consistent with demyelinating disease. The patient received a 3-day course of SoluMedrol with
improvement in vision and was discharged with a steroid taper. The patient followed up with the neurology outpatient clinic after discharge. Oligoclonal IgG bands (type 2) were positive and the patient was diagnosed with Multiple Sclerosis (MS).
Discussion
Optic neuritis is an acute, inflammatory condition of the optic nerve associated with asymmetric vision loss and eye pain. The etiology of optic neuritis, while often idiopathic, can be secondary to demyelination, self-directed antibodies, autoimmune inflammation, infections, and post-infectious/post-vaccination. Central to the pathophysiology are T and B cell lymphocytes that initiate a faulty immune response by recognizing neural autoantigens as foreign proteins. The resulting inflammatory response leads to demyelination, axonal loss, and the subsequent ocular symptomatology.
Optic neuritis classically presents in a young female (age 20-40) with symptoms of unilateral vision loss, pain with eye movement, a deficiency in color vision, and a history of a prior episode that had spontaneously improved. Optic Neuritis is a clinical diagnosis ascertained by physical exam findings such as decreased Snellen visual acuity, decreased color vision on Pelli-Robson or Vistech test, RAPD on swinging flashlight test, pain on extraocular motility exam, nerve fiber layer or central loss shown on visual field exam, and optic disc edema on dilated fundus exam (present in up to 35% of patients). The presentation of this patient generally supports the body of literature that describes epidemiology and symptomatology commonly associated with optic neuritis. A patient of female sex in her early 20s presenting with recurrent neurologic deficits and unilateral, red-denatured paints the clinical picture (Toosy et al, 2014).
For diagnostics, MRI of the brain and Orbit can help elucidate the etiology of optic neuritis. In typical Optic Neuritis, MS shows on MRI as a segment of contrast enhancement of the optic nerve and a high intensity T2 weighted lesion white matter lesions located in the periventricular, juxtacortical, infratentorial, and/or spinal cord white matter. In non-typical ON, white matter lesions may appear outside of typical locations and optic nerve enhancement is more posterior in the optic chiasm and tract. This patient underwent an MRI of the brain and orbit to validate suspicion of a CNS process that might have affected white matter structures. Asymmetric increase of T2 signal throughout the left optic nerve supports suspicion of local inflammation.
Additional testing includes CSF analysis for oligoclonal bands to confidently diagnose MS. In this patient, the oligoclonal bands detected on electrophoresis and the recurrent nature further support MS, a commonly observed etiology of optic neuritis. For non MS etiologies, VDRL and FTA-ABS can test for syphilis, antibody titers can test for lyme disease, chest x-ray and serum angiotensin-converting enzyme levels test for sarcoidosis, and ANA for Systemic lupus erythematosus and vasculitis.
The clinical evidence in this case indicates an inflammatory process, thus initial treatment of methylprednisolone was prescribed. Treatment is guided by the The Optic Neuritis Treatment Trial which evaluated the efficacy and safety of an oral placebo, oral prednisone, and IV methylprednisolone followed by oral prednisolone in treating acute ON. The 1000 mg IV methylprednisolone daily for 3 days and 11 day oral prednisone taper was found to accelerate visual recovery fastests in the first 4-6 weeks post onset but did not improve long-term outcomes. Additionally, patients who took oral steroids in conventional doses alone were found to have higher rates of recurrence of ON and are thus contraindicated in acute ON.
Overall, Optic neuritis is a complicated pathology with several etiologies and diagnostic algorithms. While multiple sclerosis is the most common typical etiology for optic neuritis, immediate treatment is the same for most causes followed by further investigation to treat the underlying cause. In this case, the patient’s clinical presentation and MRI and lab results lead towards the diagnosis and treatment of Multiple Sclerosis
References
Beck RW, Cleary PA, Anderson MM, et al. A randomized, controlled trial of corticosteroids in the treatment of acute optic neuritis. The Optic Neuritis Study Group. N Engl J Med.
1992;326(9):581-588. doi:10.1056/NEJM199202273260901
Chen JJ, Pittock SJ, Flanagan EP, Lennon VA, Bhatti MT. Optic neuritis in the era of biomarkers. Surv Ophthalmol. 2020;65(1):12-17. doi:10.1016/j.survophthal.2019.08.001
Horton JC. Disorders of the Eye. In: Jameson JL, Fauci AS, Kasper DL, Hauser SL, Longo DL,
Loscalzo J, eds. Harrison’s Principles of Internal Medicine. 20th ed. McGraw-Hill Education;
2018. Accessed January 7, 2023. accessmedicine.mhmedical.com/content.aspx?aid=1187230393
Papadakis MA, McPhee SJ, Bernstein J. Optic Neuritis. In: Quick Medical Diagnosis &
Treatment 2022. McGraw-Hill Education; 2022. Accessed January 7, 2023.
accessmedicine.mhmedical.com/content.aspx?aid=1186004205
Toosy AT, Mason DF, Miller DH. Optic neuritis. Lancet Neurol. 2014;13(1):83-99.
doi:10.1016/S1474-4422(13)70259-X
Wilhelm H, Schabet M. The Diagnosis and Treatment of Optic Neuritis. Dtsch Arztebl Int.
2015;112(37):616-625; quiz 626. doi:10.3238/arztebl.2015.0616
Diagnostic Approach to Atypical Optic Neuritis - EyeWiki. eyewiki.aao.org. Accessed January
15, 2023 https://eyewiki.aao.org/Diagnostic_Approach_to_Atypical_Optic_Neuritis#cite_note-:0-3
Demyelinating Optic Neuritis - EyeWiki. Eyewiki.aao.org. Accessed January 15, 2023.
https://eyewiki.aao.org/Demyelinating_Optic_Neuritis
Chief Complaint
A new blind spot in the right eye.
History of Present Illness
A 49-year-old male presented complaining of a new blind spot in the right eye. This symptom began 2 weeks ago described as flashes located inferotemporal in the right eye along with metamorphopsia and a scotoma. The flashes resolved and his symptoms progressed to an inferotemporal scotoma. Of note, he reported a blood pressure of 169/99 on last check which has been fluctuating with reports of low blood pressure.
Ocular History
- Zoster ophthalmicus (several years ago)
Past Medical History
- Hypertension
- Hyperlipidemia
- Asthma
- HyperIgE (Job) syndrome
- DVT after knee surgery at age 16
- Shingles/Ramsay Hunt Syndrome
Medications
- Amlodipine
- Aspirin
- Atorvastatin
- Duloxetine
- Lasix
- Pantoprazole
- Ranitidine
- Saline (ocular)
Allergies
- Ciprofloxacin
- Codeine derivatives
- NSAIDs
- Penicillin
- IV vancomycin
- HCL in dextrose
- Zosyn SOLR
Family History
- Maternal: Glaucoma, HTN/HLD, heart failure, breast cancer
- Paternal: Myocardial infarction (deceased)
Social History
- History of tobacco use (1 pack per day), current status unknown
- No alcohol use
Review of Systems
- Denies fever, chills, headache, chest pain, palpitations, shortness of breath, abdominal pain, nausea, vomiting, focal weakness, or sensation loss
Ocular Exam
Physical Exam
|
|
OD | OS |
|---|---|---|
| Visual Acuity | 20/40 | 20/50+ |
| Intraocular Pressure (mmHg) | 10 | 19 |
| Pupils | RRL no APD | RRL no APD |
| Extraocular Motility | Full | Full |
| Confrontational Visual Fields | Inferotemporal Quadrantanopia | Full |
Slit Lamp Exam
|
|
OD | OS |
|---|---|---|
| External | Normal | Normal |
| Lids and Lashes | Normal, no lesions | Normal, no lesions |
| Conjunctiva/Sclera | White and quiet | White and quiet |
| Cornea | Clear | Clear |
| Anterior Chamber | Deep and quiet | Deep and quiet |
| Iris | Round and reactive | Round and reactive |
| Lens | Clear | Clear |
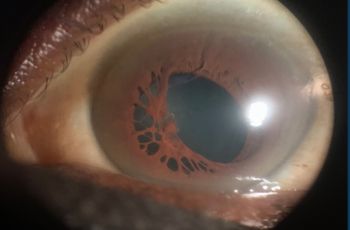
Dilated Fundus Exam
|
|
OD | OS |
|---|---|---|
| Cup to Disc | 0.25 | 0.25 |
| Optic Nerve | Pink/sharp | Pink/sharp |
| Vessels | AV nicking, plaque in vessel superior to nerve | AV nicking |
| Macula | Cotton-wool-spot superior temporal with whitening along superior macula and superior temporal arcade | Normal |
| Periphery | Flat | Flat |
| Vitreous | Clear | Clear |
Imaging
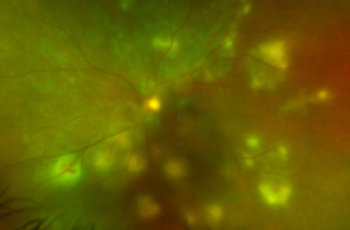
Optical Coherence Tomography (OCT) Macula (Heidelberg)
OD: distortion/thickening of inner retina
OS: normal foveal contour and thickness
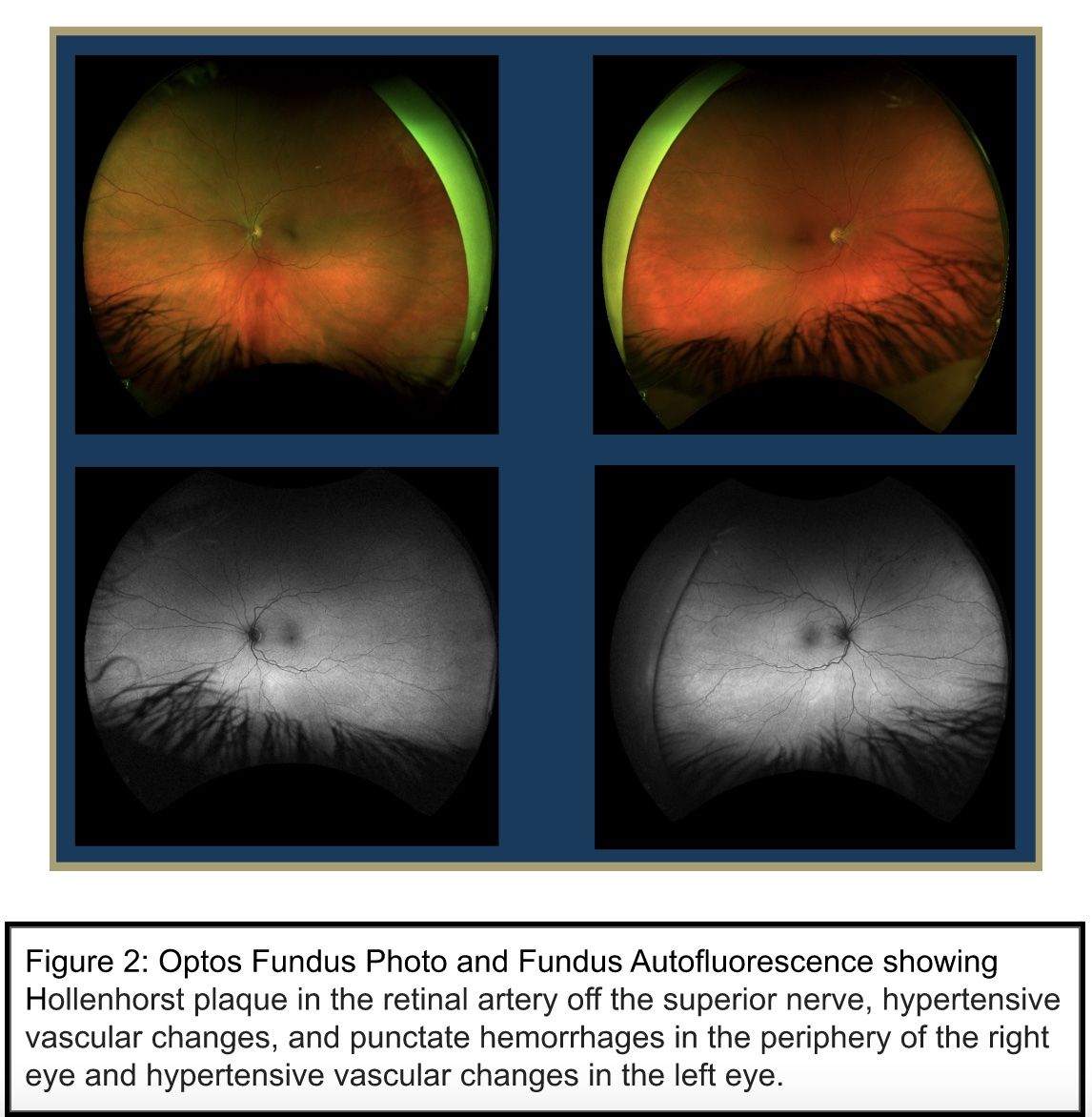
Optos Fundus Photos and Fundus Autofluorescence
OD: Hollenhorst plaque in the retinal artery superior to the optic nerve, hypertensive vascular changes, punctate hemorrhages in the periphery
OS: Hypertensive vascular changes
MRI Brain with and without contrast
Multiple small subacute intracranial infarcts within the left frontal and parietal lobes, right caudate and right inferior cerebellum and abnormal FLAIR hyperintensity with associated susceptibility hypointensity within the left parietal and occipital lobe sulci concerning for subarachnoid hemorrhage
Carotid Ultrasound
Unremarkable, minimal bilateral plaque
Trans-Thoracic Echocardiogram
Patent Foramen Ovale
Laboratory Testing
- ESR, CRP: negative
Differential Diagnosis
- Branch Retinal Artery Occlusion (BRAO)
- Transient monocular visual loss due to retinal artery vasospasm
- Hypertensive retinopathy OU
Clinical Course
This patient is a 49-year-old male who was originally referred to the ophthalmology clinic by his primary care provider for concern of retinal detachment after experiencing transient floaters and a persistent inferotemporal blind spot in the right eye. Clinical exam revealed a BRAO and he underwent a subsequent stroke work-up. Carotid ultrasound was unremarkable. Brain MRI revealed CVA with multiple subacute infarcts The patient underwent echocardiography, which revealed a patent foramen ovale (PFO). He was subsequently started on dual antiplatelet therapy. He also underwent hypercoagulability and inflammatory work-up, which were negative. He was discharged with scheduled follow-up for cardiology and neurology. The patient received a cardiology evaluation for percutaneous closure of the patent foramen ovale, but was determined to be a poor candidate for this intervention due to a recent hospitalization with sepsis. He continues to follow up with cardiology on a regular basis.
Discussion
Branch retinal artery occlusion is a cerebrovascular accident (CVA) or stroke involving the retinal vasculature. It leads to decreased blood flow to the retina and presents clinically as acute, painless monocular vision loss. On visual field testing, BRAO most commonly presents as an acute scotoma. In older adults, the etiology is often an atherosclerotic plaque/valvular emboli. In adults under 50 years of age, the etiology is often a cardiac embolic source or hypercoagulable state.
BRAO causes acute retinal ischemia and is therefore considered a vascular emergency. In this case, the patient was sent immediately to the emergency department upon diagnosis to receive a stroke work-up. This patient had pre-existing risk factors for stroke and acute coronary events. A robust work-up must be done to rule out any undiagnosed life-threatening conditions.
This patient was ultimately found to have a Patent Foramen Ovale (PFO) on imaging. PFO is a risk factor for life-threatening emboli and PFO-related BRAO have been reported in several cases in young adults (Shoebi et al. 2018). Referral to cardiology is necessary for further management of the condition.
In conclusion, BRAO is an uncommon diagnosis, especially in a patient under 50. Patients who present with retinal artery occlusion should undergo further work-up as this may ultimately reveal underlying systemic etiology. In this case, BRAO was the presenting sign that led to the diagnosis of patent foramen ovale (PFO) and the finding of multiple intracranial infarcts.
References
Biousse V, Nahab F, Newman NJ. Management of Acute Retinal Ischemia: Follow the Guidelines! Ophthalmology. 2018;125(10):1597-1607. doi:10.1016/j.ophtha.2018.03.054
Chatziralli IP, Parikakis EA, Mitropoulos PG. Undiagnosed patent foramen ovale as a rare cause for branch retinal artery occlusion. Eur J Ophthalmol. 2015;25(5):e88-90.
doi:10.5301/ejo.5000608
Greven CM, Slusher MM, Weaver RG. Retinal Arterial Occlusions in Young Adults. American Journal of Ophthalmology. 1995;120(6):776-783. doi:10.1016/S0002-9394(14)72731-X
Hayreh SS. Ocular vascular occlusive disorders: Natural history of visual outcome. Progress in Retinal and Eye Research. 2014;41:1-25. doi:10.1016/j.preteyeres.2014.04.001
Iqbal P, Shams A, Ali M, Muthanna B, Hussain T. Rare Association of Patent Foramen Ovale and Atrial Septal Aneurysm Leading to Branch Retinal Artery Occlusion in a Young Healthy Man. Cureus. 2020;12(7). doi:10.7759/cureus.8994
Wieder MS, Blace N, Szlechter MM, Shulman E, Thankenchen J, Mbekeani JN. Central retinal artery occlusion associated with patent foramen ovale: a case report and literature review. Arquivos Brasileiros de Oftalmologia. 2021;84(5). doi:10.5935/0004-2749.20210073
Acknowledgments
Case Report Authors
Case 1: Optic Neuritis
Devin Hill, MS3
Tyler Muser, MS2
Case 2: Branch Retinal Artery Occlusion
Sahak Hovsepian, MS3
Shaleen Arora, MS2
Resident Editors
Masumi Asahi, DO
Braedon Murdock, MD
Will Foos, MD
Attending Reviewer
David Belyea, MD MBA
Editors in Chief
Jason Dossantos, MS3
Julie Thomasian, MS4